Access to Care Rankings
The Access Ranking indicates how much access to mental health care exists within a state. The access measures include access to insurance, access to treatment, quality and cost of insurance, access to special education, and workforce availability. A high Access Ranking indicates that a state provides relatively more access to insurance and mental health treatment.
The 9 measures that make up the Access Ranking include:
- Adults with AMI who Did Not Receive Treatment
- Adults with AMI Reporting Unmet Need
- Adults with AMI who are Uninsured
- Adults with Disability who Could Not See a Doctor Due to Costs
- Youth with MDE who Did Not Receive Mental Health Services
- Youth with Severe MDE who Received Some Consistent Treatment
- Children with Private Insurance that Did Not Cover Mental or Emotional Problems
- Students Identified with Emotional Disturbance for an Individualized Education Program
- Mental Health Workforce Availability
Access to Care Map
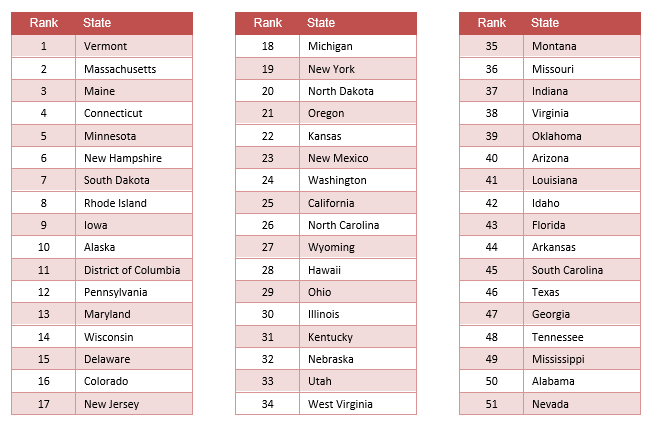
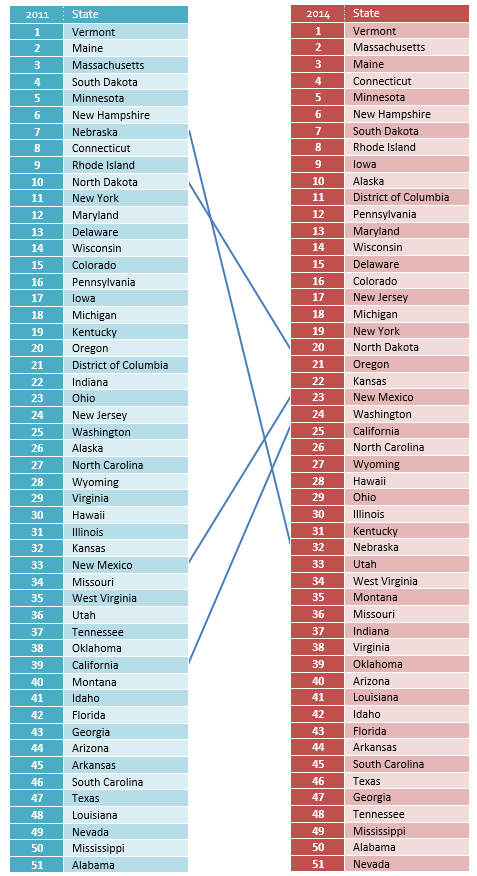
Access to Care Ranking - 2011 vs. 2014
 State and local level policies have the biggest impact on access to mental health care. Changes in these rankings may reflect policy changes that support constituencies who suffer from mental health problems. For example, states who passed laws supporting implementation of mental health parity laws and the Affordable Care Act show improvements in access to insurance rates. Those states that took aggressive policy changes, such as the implementation of The Mental Health Services Act in California, resulted in significant changes in access to care. The connecting lines point to several changes among those states that have significant movement in ranking. A lack of movement at the top could indicate long term commitment towards better mental health policies. While lack of movement at the bottom indicates continued neglect of the mental health needs of constituencies. States can compare policies among other better performing states of equivalent size, geography, culture, or political affiliation to identify potential policy changes to improve their numbers and rankings.
State and local level policies have the biggest impact on access to mental health care. Changes in these rankings may reflect policy changes that support constituencies who suffer from mental health problems. For example, states who passed laws supporting implementation of mental health parity laws and the Affordable Care Act show improvements in access to insurance rates. Those states that took aggressive policy changes, such as the implementation of The Mental Health Services Act in California, resulted in significant changes in access to care. The connecting lines point to several changes among those states that have significant movement in ranking. A lack of movement at the top could indicate long term commitment towards better mental health policies. While lack of movement at the bottom indicates continued neglect of the mental health needs of constituencies. States can compare policies among other better performing states of equivalent size, geography, culture, or political affiliation to identify potential policy changes to improve their numbers and rankings.
Change Over Time, 2011-2014
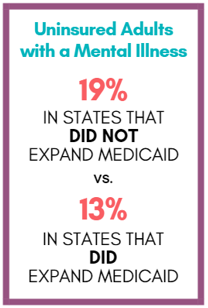
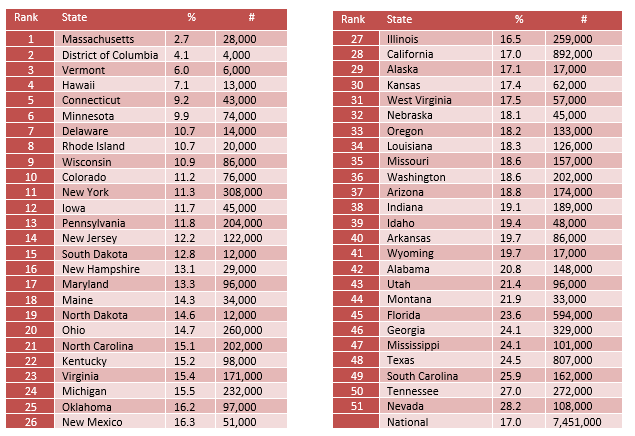
Adults with AMI who are Uninsured
17% (over 7.5 million) of adults with a mental illness remain uninsured.
With a national focus on health care access, the uninsured rate is improving.
In 2011, 19% of adults with a mental illness were uninsured.
Alabama, Louisiana, Oklahoma, and New Mexico had the largest increase in access to mental health coverage among adults.
Unfortunately, having insurance coverage does not mean access needed treatment.
56.5% of adults with mental illness received no past year treatment, and for those seeking treatment, 20.3% continue to report unmet treatment needs.
The state prevalence of uninsured adults with mental illness ranges from 2.7% in Massachusetts to 28.2% in Nevada.
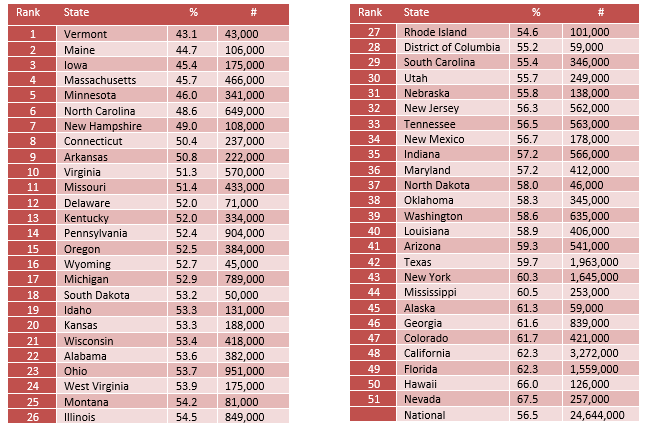
Adults with AMI who Did Not Receive Treatment
56.5% of adults with a mental illness received no treatment. Lack of access to treatment is slowly improving. In 2011, 59% of adults with a mental health problem did not receive any mental health treatment.
Reasons for not receiving treatment can be individual or systemic.
It is often the case that it takes time for people to recognize that what they are experiencing are symptoms of a mental health problem. 84% of the time between first symptoms and first treatment is spent not recognizing the symptoms of mental illness.6
Providing people with accessible and easy screening tools or encouraging primary care physicians to screen and ask about mental health problems are necessary in reducing untreated mental illness.
The state prevalence of untreated adults with mental illness ranges from 43.1% in Vermont to 67.5% in Nevada.
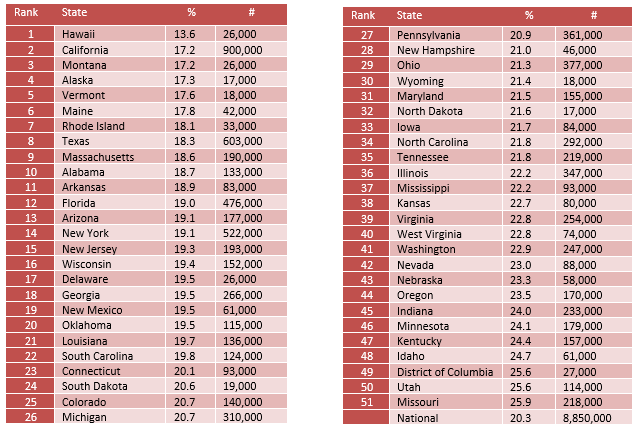
Adults with AMI Reporting Unmet Need
One out of five (20.3%) adults with a mental illness report they are not able to get the treatment they need.
States with the highest levels of unmet need (bottom 10) are 1.6 times more likely to have people report unmet need.
Unlike the number of people with mental illness who did not receive treatment, the individuals who are reporting unmet need are seeking treatment and facing barriers to getting the help they need.
Once a person recognizes that they may have a mental health problem, finding support especially the right kind of support is often difficult. Several systemic barriers to accessing care include:
- Lack of insurance or inadequate insurance
- Lack of available treatment providers
- Lack of available treatment types (inpatient treatment, individual therapy, intensive community services)
- Insufficient finances to cover costs – including, copays, uncovered treatment types, or when providers do not take insurance.
The state prevalence of adults with AMI reporting unmet treatment needs ranges from 13.6% in Hawaii to 25.9% in Missouri.
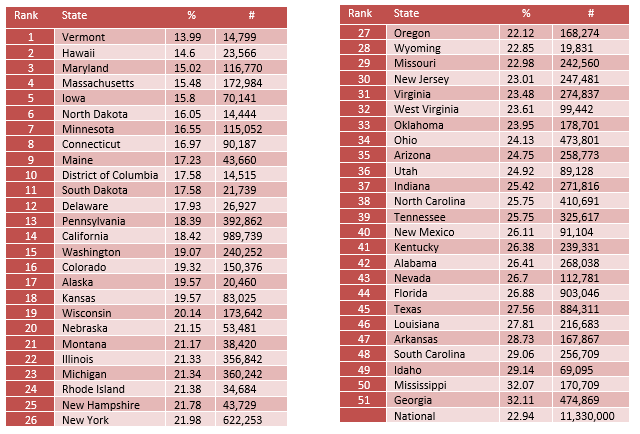
Adults with Disability Who Could Not See a Doctor Due to Costs
22.94% of adults with a disability were not able to see a doctor due to costs. The inability to pay for treatment, due to high treatment costs and/or inadequate insurance coverage remains a barrier for individuals despite being insured.
People with mental health problems have a 2.5 to 7 times greater odds of facing barriers to medical care and 50% of adults who have untreated need, didn’t receive treatment because of costs. These barriers include not having access to a primary care physician, not being able to get needed medical care, not having accesses to needed medication, and delayed medical treatment because of costs.2
The prevalence of adults with disability who couldn’t see a MD due to cost ranges from 13.99% in Vermont to 32.11% in Georgia.
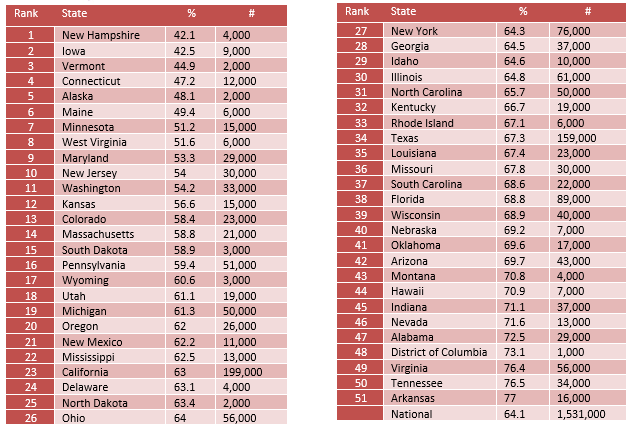
Youth with MDE who Did Not Receive Mental Health Services
64.1% of youth with major depression do not receive any mental health treatment.
That means that 6 out of 10 young people who have depression and who are most at risk of suicidal thoughts, difficulty in school, and difficulty in relationships with others do not get the treatment needed to support them.
The state prevalence of untreated youth with depression ranges from 42.1% in New Hampshire to 77.0% in Arkansas.
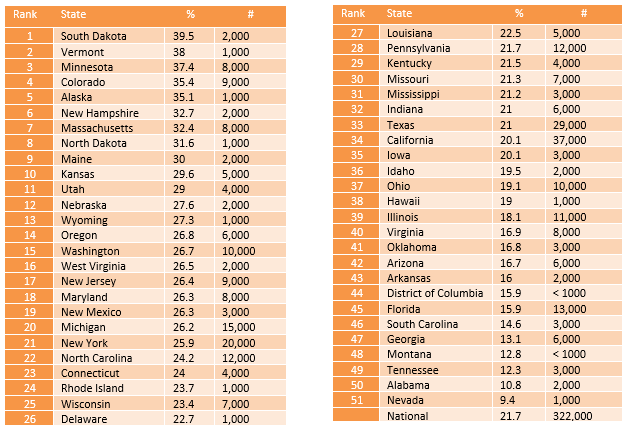
Youth with Severe MDE who Received Some Consistent Treatment
Nationally, only 21.7% of youth with severe depression receive some consistent treatment (7-25+ visits in a year).
Even among youth with severe major depression, 62.6% did not receive any mental health treatment.
The state prevalence of youth with severe depression who received some outpatient treatment ranges from 39.5% in South Dakota to 9.4% in Nevada.
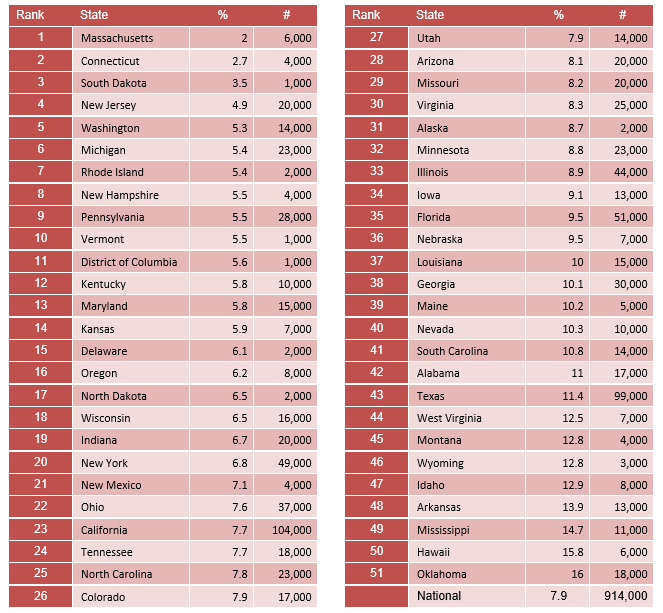
Children with Private Insurance that Did Not Cover Mental or Emotional Problems
Children and youth are more likely to have insurance coverage compared to adults.
7.9% of youth had private health insurance that did not cover mental or emotional problems.
Kansas, Louisiana, Arizona, and South Carolina saw the largest increase in access to mental health coverage among children.
Reduction in uncovered mental health care among those states are:
- Kansas – 11.3% in 2011 to 5.9% in 2014
- Louisiana – 14.7% in 2011 to 10.0% in 2014
- Arizona – 12.5% in 2011to 8.1% in 2014
- South Carolina – 14.9% in 2011 to 10.8% in 2014
Like adults, having insurance coverage does not mean access needed treatment.
The percentage of youth with severe depression who received insufficient treatment (less than 6 or no sessions of treatment) in each of the above states are:
- Kansas – 70.4%
- Louisiana – 77.5%
- Arizona – 83.3%
- South Carolina – 85.4%
The state prevalence of children lacking mental health coverage ranges from 2.0% in Massachusetts to 16.0% in Oklahoma.
Students Identified with Emotional Disturbance for an Individualized Education Program
.771% of students are identified as having an Emotional Disturbance (ED) for an Individualized Education Program (IEP).
The term “Emotional Disturbance” is used to define youth with a mental illness for purposes of an IEP. Often times youth with emotional or mental health problems are identified as having other issues rather than an emotional or mental health problem. In such cases, it is unclear whether their mental health problems are taken into consideration in planning for appropriate educational modifications and accommodations in their IEP.
The rate for this measure is shown as a rate per 1,000 students.
The calculation was made this way for ease of reading. Unfortunately, doing so hides the fact that the percentages are significantly lower.
If states were doing a better job of identifying whether youth had emotional difficulties that could be better supported through an IEP – the rates would be closer to 8% instead of .8 percent.
The state rate of students identified as having an emotional disturbance for and IEP ranges from 26.35 per 1,000 students in Vermont to 1.82 per 1,000 students in Arkansas.

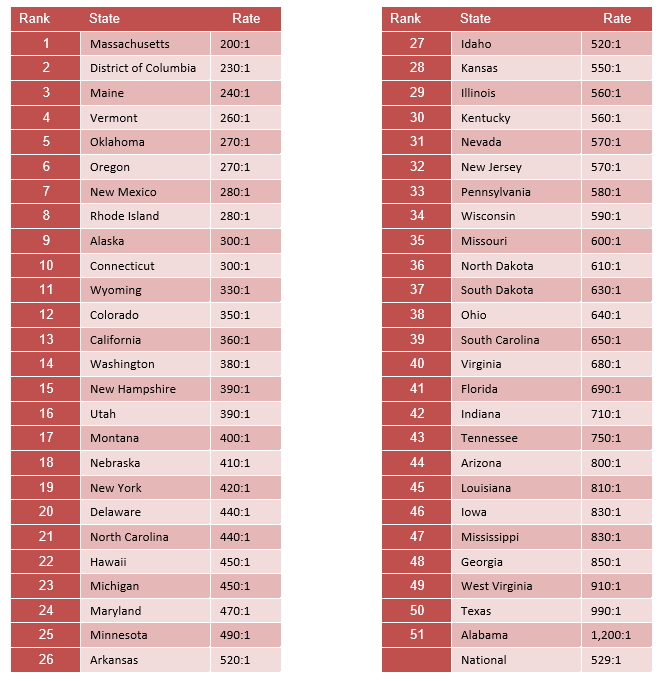
Mental Health Workforce Availability
Nationally, there is one mental health provider for every 529 individuals. The term mental health provider includes: psychiatrists, psychologists, licensed clinical social workers, counselors, marriage and family therapists and advanced practice nurses specializing in mental health care.
The workforce shortage among specialized mental health professionals – such as child psychiatrists or forensic specialists are even higher. There are an estimated 8,300 child psychiatrists across the county compared to over 15 million youths with mental health disorders. (http://www.aacap.org/aacap/resources_for_primary_care/Workforce_Issues.aspx)
Over 4,000 areas across the US are considered mental health professional shortage areas, leaving people to travel hours or across state lines to access services. (https://bhw.hrsa.gov/shortage-designation)
To make matters worse, the addition of low reimbursement rates combined with a limited number of providers and high demand for help means that many do not accept insurance, forcing families and individuals to pay high out-of-pocket fees or go without care.
Peer support specialists, workforce development programs, telehealth, or primary care models like Collaborative Care are possible solutions to the significant mental health workforce gap in the states.
The state rate of mental health workforce ranges from 200:1 in Massachusetts to 1,200:1 in Alabama.