Depression Support and Advocacy
Depression Information and Resources
- Basic Facts About Depression
- Depression Test
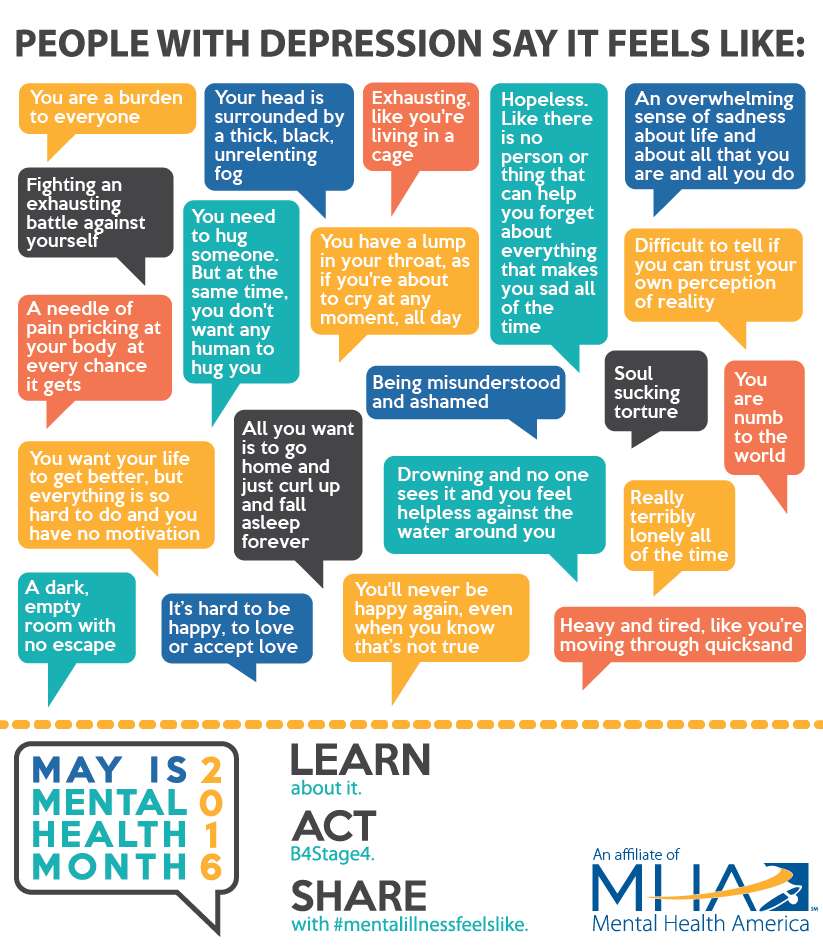
- What Depression Feels Like
- Causes of Depression
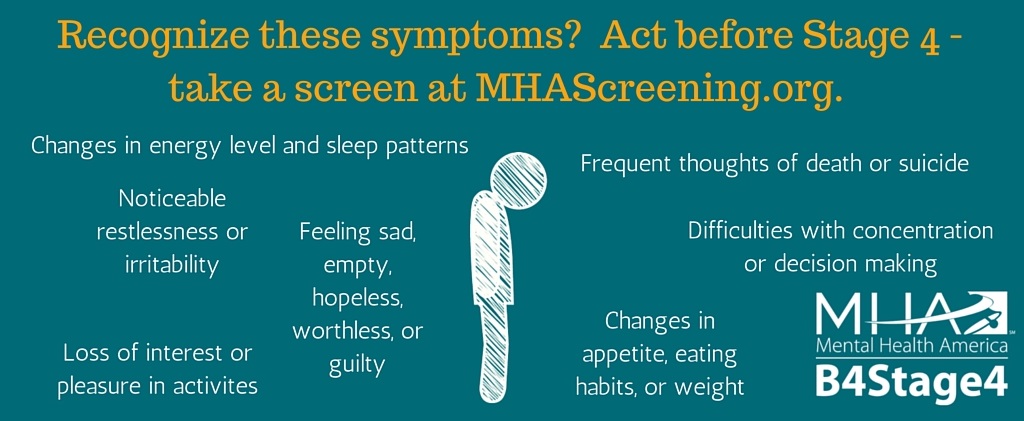
- Symptoms of Depression
- Kinds of Depression
- Treatment for Depression
- Other Mental Health Screens
- Finding Local Resources
- Getting Involved in Advocacy
- Other Depression Information
Basic Facts About Depression
- Major depression is one of the most common mental illnesses, affecting 6.7% (more than 16 million) of American adults each year.[1]
- Depression causes people to lose pleasure from daily life, can complicate other medical conditions, and can even be serious enough to lead to suicide.
- Depression can occur to anyone, at any age, and to people of any race or ethnic group. Depression is never a "normal" part of life, no matter what your age, gender or health situation.
- While the majority of individuals with depression have a full remission of the disorder with effective treatment, only about a third (35.3%) of those suffering from severe depression seek treatment from a mental health professional.[2] Too many people resist treatment because they believe depression isn't serious, that they can treat it themselves or that it is a personal weakness rather than a serious medical illness.
Sadness or Something More?
If you're not sure if you have depression, take a depression screen.
See What Others Are Saying About Depression
Visit #mentalillnessfeelslike and engage in the power of sharing
 |
 |
Our Mental Health Month toolkit has information on depression and self help tools you can use at home.
 |
 |
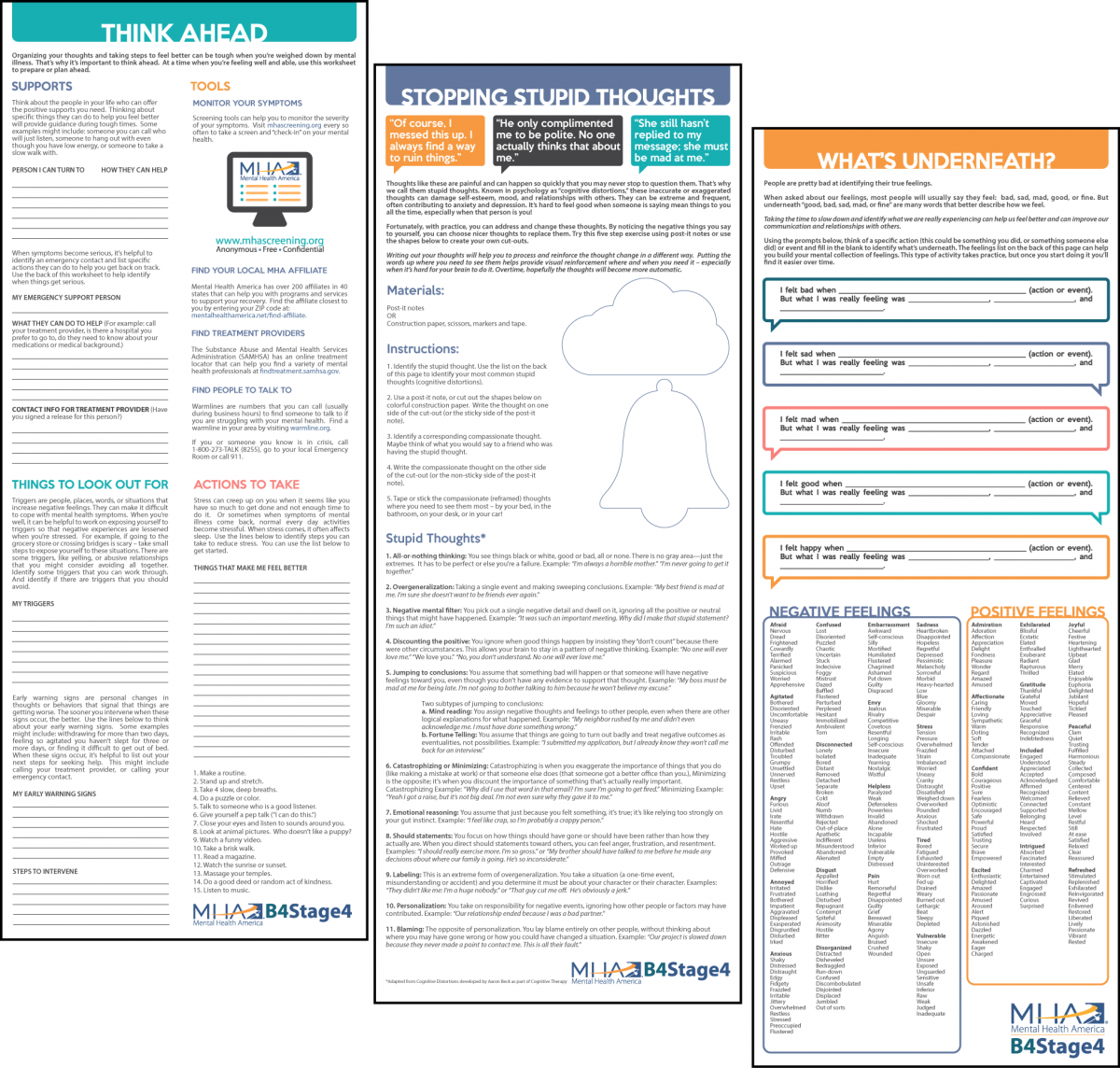 |
Download the Toolkit |
View the Infographic |
Check out the Self-Help Tools |
What Are the Causes of Clinical Depression?
Many things can contribute to clinical depression. For some people, a number of factors seem to be involved, while for others a single factor can cause the illness. Oftentimes, people become depressed for no apparent reason.
Biological - People with depression may have too little or too much of certain brain chemicals, called "neurotransmitters." Changes in these brain chemicals may cause or contribute to depression.
Cognitive - People with negative thinking patterns and low self-esteem are more likely to develop clinical depression.
Gender - More women experience depression than men.[3] While the reasons for this are still unclear, they may include the hormonal changes women go through during menstruation, pregnancy, childbirth and menopause. Other reasons may include the stress caused by the multiple responsibilities that women have.
Co-occurrence - Depression is more likely to occur along with certain illnesses, such as heart disease, cancer, Parkinson's disease, diabetes, Alzheimer's disease, Multiple Sclerosis and hormonal disorders.
Medications - Side effects of some medications can bring about depression.
Genetic - A family history of depression increases the risk for developing the illness. Some studies also suggest that a combination of genes and environmental factors work together to increase risk for depression. [4]
Situational - Difficult life events, including divorce, financial problems or the death of a loved one can contribute to depression.
What Are the Symptoms of Clinical Depression?
The following are symptoms that are often experienced with depression. In order to have clinical depression, you would have to experience 5 or more of these symptoms for a 2 week period and because of the symptoms have caused trouble in life - for example having trouble in school or work. Sometimes life factors like losing a job, becoming sick, or losing a loved one can trigger sadness. A mental health professional or support person could help you determine how to make sense of your symptoms and explore treatment options.
- Persistent sad, anxious or "empty" mood
- Loss of pleasure and interest in activities once enjoyed, including sex
- Sleeping too much or too little, middle of the night or early morning waking
- Reduced appetite and weight loss, or increased appetite and weight gain
- Restlessness, irritability
- Persistent physical symptoms that do not respond to treatment (such as chronic pain or digestive disorders)
- Difficulty concentrating, remembering or making decisions
- Fatigue or loss of energy
- Feeling guilty, hopeless or worthless
- Thoughts of suicide or death?
What Are the Different Kinds of Depression?
Depressive Disorders are a category of mood disorders that involve extended periods of feeling extremely low and disrupt a person’s ability to enjoy life. Some of the most common Depressive Disorders include:
Major Depressive Disorder (Clinical Depression); a mental health condition characterized by an inescapable and ongoing low mood often accompanied by low self-esteem and loss of interest or pleasure in activities that a person used to find enjoyable. To meet the criteria for Major Depressive Disorder (MDD), symptoms must be present nearly every day for at least 2 weeks. MDD is also often referred to as Major Depression.
Persistent Depressive Disorder; refers to a longer lasting form of depression. While Major Depressive Disorder is diagnosed if an individual experiences symptoms for at least 2 weeks, Persistent Depressive Disorder is used when symptoms of depression are present on most days for at least two years, but do not reach the severity of a major depressive episode. (Prior to the release of the DSM-5 this was more commonly known as Dysthymia.)
Post-Partum Depression; depression that starts after child birth and lasts at least two weeks, up to a year.
Premenstrual Dysphoric Disorder; a severe form of Pre-Menstrual Syndrome that is diagnosed when a woman experiences severe symptoms of depression, tension, and irritability in the week prior to menstruation. While it isn’t uncommon for most women to experience emotional and physical changes prior to menstruation, women who meet criteria for PMDD experience changes that impact their lives in more profound ways.[5]
Seasonal Affective Disorder; a mood disorder involving symptoms of depression associated with varying levels of sunlight during fall and winter months which subsides during spring and summer.
Depression is also a feature of Bipolar Disorder.
What Are the Treatments for Depression?
Depression is very treatable, with the overwhelming majority of those who seek treatment showing improvement.The most commonly used treatments are antidepressant medication, psychotherapy or a combination of the two.
- Peer Support – Peer Support refers to receiving help from individuals who have suffered from similar experiences.
- Support Group – A support group is a group meeting where members guide each other towards the shared goal of recovery. Support groups are often comprised of nonprofessionals, but peers that have suffered from similar experiences.
- Psychotherapy – Psychotherapy is the therapeutic treatment of mental illness provided by a trained mental health professional. Psychotherapy explores thoughts, feelings, and behaviors, and seeks to improve an individual’s well-being. Psychotherapy paired with medication is the most effective way to promote recovery. Examples include: Cognitive Behavioral Therapy, Exposure Therapy, Dialectical Behavior Therapy, etc.
- Medication – Medication does not outright cure mental illness. However, it may help with the management of symptoms. Medication paired with psychotherapy is the most effective way to promote recovery.
- Case Management – Case management coordinates services for an individual with the help of a case manager. A case manager can help assess, plan, and implement a number of strategies to facilitate recovery.
- Complementary & Alternative Medicine – Complementary & Alternative Medicine, or CAM, refers to treatment and practices that are not typically associated with standard care. CAM may be used in place of or addition to standard health practices.
- Self Help Plan – A self-help plan is a unique health plan where an individual addresses his or her condition by implementing strategies that promote wellness. Self-help plans may involve addressing wellness, recovery, triggers or warning signs.
- Hospitalization – In a minority of cases, hospitalization may be necessary so that an individual can be closely monitored, accurately diagnosed or have medications adjusted when his or her mental illness temporarily worsens.
Learn more about therapy, how to find therapy, and medication.
The choice of treatment depends on the pattern, severity, persistence of depressive symptoms and the history of the illness. As with many illnesses, early treatment is more effective and helps prevent the likelihood of serious recurrences. Depression must be treated by a physician or qualified mental health professional.
For some people, depression can be very stubborn to treat and may require additional treatment options. Learn more here - Dealing with Treatment-resistant Depression: What to Do When Treatment Doesn't Seem to Work.
Other Screening Tools
It isn't uncommon for people to struggle with a mixture of symptoms. Many people for example find that they have both sadness and overwhelming anxiety.
If you're interested in taking other mental health screens, visit MHAScreening.org or click on the image below
Finding Local Resources
MHA Affiliate Network
The MHA Affiliate Network is comprised of more than 200 mental health organizations that work to influence public policy to assure access to fair and effective treatment for the millions of Americans suffering from mental health conditions. MHA affiliates bring together mental health consumers, caregivers, advocates and service providers for collaboration and action to inform, support and enable mental wellness, and emphasize recovery from mental illness. Each MHA affiliate offers a unique blend of programs and mental health services through public education, advocacy, information and referral, peer support, rehabilitation services as well as socialization and housing services to those confronting mental health challenges.
To find an MHA affiliate in your area, click here.
SAMHSA Treatment Locator
The SAMHSA Substance Abuse Treatment Facility Locator and the SAMHSA 24/7 Treatment and Referral line at 1.800.662.4357 provide referrals to alcohol, substance abuse and dual diagnosis treatment facilities, including facilities that offer sliding scale fees and other special payment arrangements. Dual diagnosis services provide integrated treatment for individuals who have both an alcohol or substance abuse problem and a mental illness. Use the detailed search option on the left hand side of the page to find the facilities that most closely match your needs.
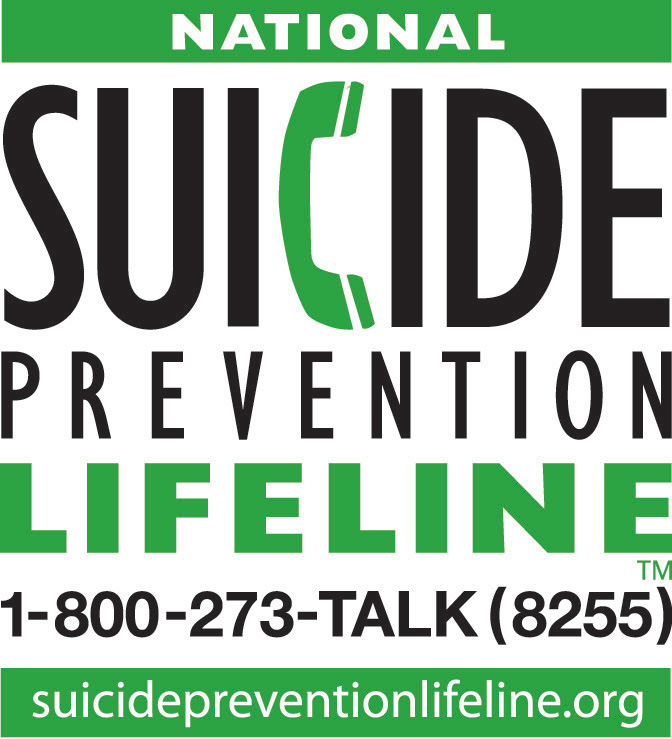
Crisis Hotline
The National Suicide Prevention Lifeline's 24 hour toll-free crisis hotline, 1.800.273.TALK (1.800.273.8255) can put you into contact with your local crisis center that can tell you where to seek immediate help in your area.

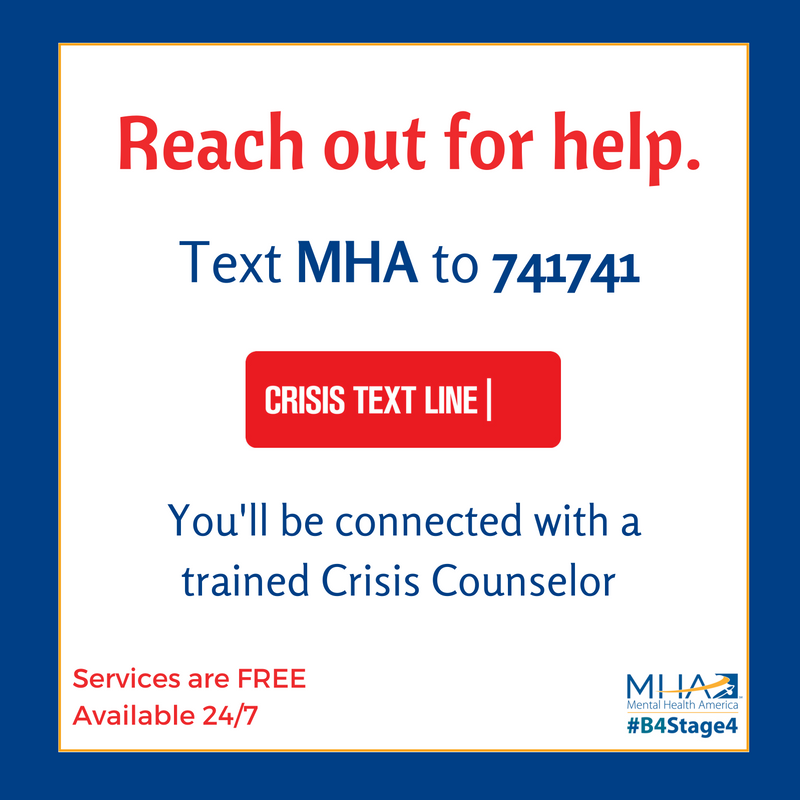
Crisis Text Support
The Crisis Text Line provides text-based crisis support from any cell phone enabled to send and receive text messages. Individuals are connected with a Trained Crisis Counselor and can chat via text 24 hours a day, 7 days a week. Individuals send MHA to 741-741 to get connected and start the text-based conversation.
Interested in Getting Involved
Join Our Advocacy Network
Join our movement by signing up for Action Alertsor learn more about #B4Stage4.
You can also join the movement on social media – our Facebook page has more than 127,000 fans and our Twitter profile has more than 69,000 followers!
MHA Partnerships
MHA National works with a comprehensive network of partners in order to effectively address the needs of communities across the U.S. Together, with our partners, we leverage our combined knowledge and resources to effect change at the individual and societal levels. Our partnerships range in focus, and are targeted collaborations aimed at reaching a variety of stakeholder groups often resulting in co-branded, tailored content and messaging for promoting topics of mutual interest.
To learn more about our current partners and partnering with MHA, click here.
MHA Associate Members
Associate membership enables organizations with the unique opportunity to become part of MHA’s diverse network. Membership is available to any private and non-profit entity that shares and supports MHA’s mission and vision.Aligning with our network increases visibility and knowledge of member services and resources to a broad spectrum of MHA stakeholders.
To learn more about benefits of membership or to apply, click here.
Other Links
- Co-occurring Disorders and Depression
- Dealing with Treatment-resistant Depression: What to Do When Treatment Doesn't Seem to Work
- Depression and African Americans
- Children's Depression Checklist
- Depression in Teens
- Depression in Older Adults
- Depression in Older Adults: More Facts
- Depression in the Workplace
- Depression in Women
- Infographic: Life with Depression
- Mood Disorders
- Postpartum Disorders
- Seasonal Affective Disorder (SAD)
- Take a Depression Screening
- Breaking Down the Myths About Depression PDF
- Staying Well When You Have a Mental Illness PDF
En Espanol:
For Community Organizations
Sources
[1] Substance Abuse and Mental Health Services Administration, Results from the 2013 National Survey on Drug Use and Health: Mental Health Findings, NSDUH Series H-49, HHS Publication No. (SMA) 14-4887. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014.
[2] Pratt LA, Brody DJ. Depression in the U.S. household population, 2009–2012. NCHS data brief, no 172. Hyattsville, MD: National Center for Health Statistics. 2014.
[4] Tsuang MT, Bar JL, Stone WS, Faraone SV. Gene-environment interactions in mental disorders. World Psychiatry, 2004 June; 3(2):73–83.
[5] American Psychiatric Association. (2014). Understanding Mental Disorders: Your Guide to DSM-5. Washington, DC: American Psychiatric Publishing.